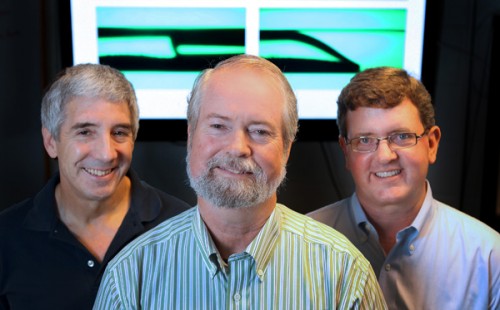
When Dr. Rick Haselton, Professor of Biomedical Engineering at Vanderbilt University, visited a hospital in India, he was shocked at the inefficiency of health care. Since rural areas did not possess the necessary tools, a patient would have to trek hundreds of miles and spend days waiting in a crowded public hospital — all for a simple blood test. This problem occurs in other countries, too, as the medical resources of developing countries often remain meager at best. However, thanks to research by Haselton and other scientists, new cheap yet ingenious devices have begun to mitigate those shortcomings. In 2011, Haselton and his colleagues at Vanderbilt developed the “Extractionator,” a novel and relatively simple apparatus for diagnosing malaria.
A mosquito-borne disease that kills more than half a million people per year, malaria traditionally is diagnosed by examining blood samples under microscopes in hospital labs. This makes diagnoses particularly tricky in places like Africa, where access to well-equipped hospitals is limited. Though increased global investment in malaria prevention has helped fund networks of health workers and provide products like insecticide-treated nets, a method of quickly detecting malaria has remained out of reach until recently.
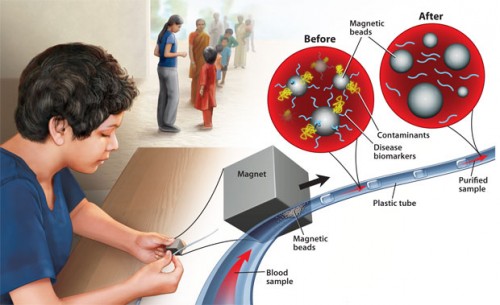
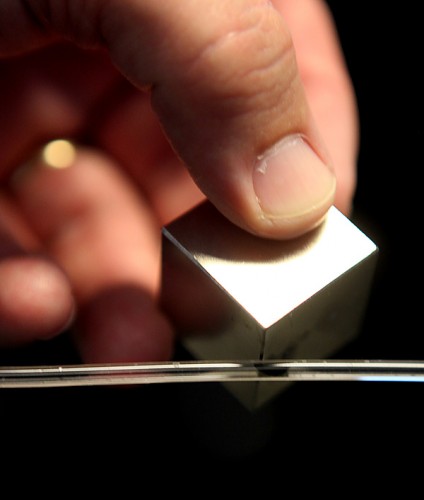
Enter the Extractionator, which was funded by a $1 million grant from the Bill & Melinda Gates Foundation for the development of a “low tech, high science” blood testing device. Haselton’s initial design was remarkably simple. First, the patient’s blood sample was stored in a thin tube that contained tiny magnetic beads, each coated with nickel. The nickel could then bind to a specific protein that is produced by malaria, called histidine-rich protein 2. This way, a large magnet sliding along the length of the tube could remove the beads and any bound malarial proteins from the rest of the blood.
As an individual bead with bound malarial proteins moved through the tube, chemicals in the successive chambers would remove any contaminating molecules from the bead-protein combination. Further down, the protein is separated from the bead in a chamber that binds a salt to the nickel. The final product, the purified protein, is placed on a diagnostic chip that could detect the protein. In this way, the Extractionator could determine whether a blood sample contains malaria.
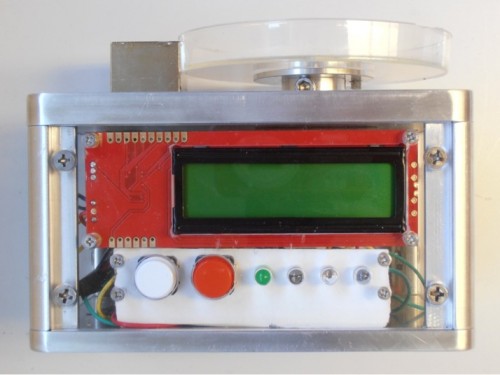
The fully automated, new, and improved Extractionator that Haselton and his researchers market today is even easier to use: The only human-operated step is insertion of the blood sample. Not only is it convenient, but the Extractionator is also very accurate in its diagnosis. As David Wright, one of the professors working on the project, explained to the Vanderbilt press office, “[Current] tests are not very effective because they lack sensitivity… the Extractionator could ensure that only the people who have malaria are treated.”
While Haselton’s device currently identifies malaria only, this is still a major achievement. Now, instead of traveling for days to reach the nearest hospital, people can use the Extractionator to test their blood for malaria. Furthermore, the technology behind the device can be used to detect other pathogens as well by coating the magnetic beads with different substances. Tuberculosis DNA, for example, binds to silicon. By coating the beads with silica instead of nickel, the Extractionator could be used to determine whether someone has been infected by tuberculosis. “In the future we want to develop a coating that will target 20 different targets in a single sample,” said Dr. Ray Mernaugh, the third principal investigator on the project, in an interview with Vanderbilt.
Haselton’s device is one of several low-cost, blood-based tests that can be used in developing countries. Dr. Wei Shen, a chemical engineer at Monash University in Melbourne, Australia, designed a low-cost, easy to use blood type test which, like the Extractionator, can be interpreted by non-professionals. He indented a piece of paper with the letters A, B, and O and filled the letters with the corresponding antibodies. Because a specific blood type carries an antigen that reacts and bonds with the corresponding antibody, the blood clumps up if the antigen and antibody are a match. Hence, if type A blood is introduced, it binds to the antibody contained in the letter A, reporting the blood type.
Haselton and Shen’s devices place the power of diagnosing disease in the hands of the patients themselves, saving them time, effort, and money. As their availability grows more widespread, people in many developing countries will no longer have to travel far and wait in long lines to receive simple blood tests for crippling diseases like malaria. Hopefully, as scientists start to do research in this field, devices like these will proliferate, helping to solve the world’s health problems.
