Over a century has passed since German physician Dr Alois Alzheimer documented the case of August Deter, a patient whose misunderstood and senseless behavior earned her admittance at a mental institution in Frankfurt in 1901. When Dr. Alzheimer asked for her name, August responded with the now eminent phrase, “I have lost myself.”
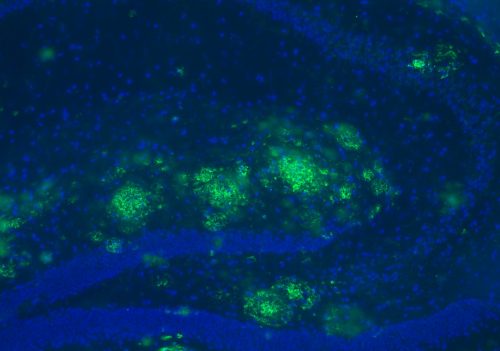
August would be the first patient diagnosed with Alzheimer’s Disease. After her death, Dr. Alzheimer examined her brain and reported the presence of peculiar alterations in August’s brain tissue which would later be called plaques and tangles. These changes are now considered hallmarks of a disease which contribute to the progressive decline in cognitive function of over five million people in the United States alone.
Researchers in the Strittmatter lab at the Yale School of Medicine used a new drug to restore the memory and learning abilities of mice with Alzheimer’s. Unlike other Alzheimer’s drugs that are sometimes linked to adverse side-effects, this drug, called SAM, specifically targets the proteins linked to the disease without affecting essential proteins in the brain.
A Sticky Disease
Plaques are sticky clusters made up of proteins called beta-amyloid that accumulate between nerve cells in the brain. Recent evidence suggests that small aggregates of beta-amyloid plaques are more damaging than the massive plaques themselves. These aggregates, called oligomers, cluster in synapses, the small gaps separating neurons of the brain, and block cell-to-cell communication. When synapses are disrupted, neurons cannot send electrical signals to each other, a dysfunction that ultimately contributes to the loss of memory and brain function characteristic of Alzheimer’s disease.
On a molecular level, research has shown that the interaction between two particular proteins leads to Alzheimer’s disease. These two proteins are called cell-surface glycoprotein (PrP) and metabotropic glutamate receptor 5 (mGluR5). The interaction between these two proteins relays neurotoxic signals across the brain, damages synapses and drains the brain’s cognitive capacity. Beta-amyloid peptides play a role in this process by strengthening the disease-causing interaction between PrP with mGluR5.
The catch, however, is that these proteins also serve important roles in the normal functioning of the body. GluR5, for example, is a receptor found on membranes of neurons which interacts with glutamate, a chemical messenger that relays signals across the synapses of neurons. Glutamate plays an essential role in a wide range of neural functions including learning, memory, and synaptic plasticity, the ability of synapses in the brain to adapt to new information and strengthen over time. The more closely? neurons are “wired” together at their synapses, the more robust the brain’s ability to communicate between neurons will be.
Introducing SAM
Alzheimer’s drugs that block glutamate interaction with mGluR5 have been shown to trigger visual hallucinations, insomnia, and cognitive dysfunction. As a result, designing an Alzheimer’s drug that specifically targets the interaction between beta-amyloid, PrP, and mGluR5 while leaving glutamate signaling undamaged has the goal of researchers for many years. “A few years ago, we did an experiment with a drug that blocks mGluR5, and it ameliorated some Alzheimer’s conditions but the drug also blocks glutamate,” Stephen Strittmatter said. “What we really need, however, is a drug that stops Alzheimer’s but preserves the normal physiology of glutamate.”
The researchers contacted the American pharmaceutical company Bristol Myers Squibb and requested a schizophrenia drug called SAM. The researchers noticed that SAM acted on the same mGluR5 pathway they were studying and predicted that SAM would have an effect on their Alzheimer’s mice. Encouragingly, the researchers found that SAM blocks the interaction of a beta-amyloid with PrP and mGluR5 but leaves glutamate signaling unaffected in mice. To determine this, the researchers measured the amount of calcium ions released inside the neurons, since glutamate signaling is known to be involved with the release of that ion. Because SAM did not alter calcium levels in the brain, the researchers concluded that SAM does not disturb glutamate signaling. “We found that SAM blocks one type of signaling through GluR5 but maintains another: glutamate signaling. It stops the pathology but leaves the physiology,” Strittmatter said.
Like most Alzheimer’s drugs, SAM binds to PrP and mGluR5 in a way that changes the overall shape of the group. This prevents beta-amyloid peptides from sticking to the group and forming the toxic protein clusters that damage synapses. Further, the researchers showed that SAM does not alter the strength of signals transmitted between neurons in mice brains. Thus, SAM selectively targets the disease-causing mechanism of Alzheimer’s while leaving normal functions undamaged.
Maze Trials
The researchers examined whether SAM could ameliorate memory deficits in mice models of Alzheimer’s. The mice’s first task was a water maze. “When the mice are young and they don’t yet have accumulated amyloid in the brain, they can learn tasks like how to figure out a maze, but as the mice age and accumulate amyloid and lose synapses, they become unable to learn,” Strittmatter said. The Alzheimer’s mice, the Alzheimer’s mice treated with SAM, and the healthy mice were all given the task to navigate the same maze and find a platform submerged in a pool.
For the next three days, the mice became familiarized with the layout of the maze. The researchers positioned the mice at 24 different starting points but kept the location of the platform constant in an effort to enforce learning. Following the third day of training, the mice were put to the test. Whereas the Alzheimer’s mice were slow to reach the platform, Alzheimer’s mice treated with SAM demonstrated significant improvement, arriving to the platform only a few seconds behind the healthy mice.
Then, the researchers removed the platform from the pool and observed how the mice navigated the maze. The healthy mice spent a significant amount of time swimming around the zone that the platform used to be located, showing that they had successfully learned to correlate the general location of the platform with safety. In contrast, the Alzheimer’s mice swam around the pool at random, indicating that they didn’t “remember” where the platform should have been. Mice treated with SAM exhibited restored memory and spent a comparable amount of time in the platform zone to the healthy mice. Accordingly, SAM successfully rescued memory and learning deficits in Alzheimer’s mice.
Through the Mouse Hole
“Another innate behavior of [mice] … is that they scurry around the room and jump into a dark hole in the corner,” said Santiago Salazar, a graduate researcher in the Strittmatter lab and second author of the paper. This natural behavior spurred the researchers to design another experiment to test the power of SAM in recovering the learning and memory aptitudes of mice. The researchers divided a chamber into a well-lit side and a dark side. On the dark side, they plated the floor with a surface that delivered a mild shock to the mice.
The mice were placed in the light chamber for 90 seconds before the door separating the light and dark chambers was opened. As expected, the mice initially jumped through the hole to reach the dark chamber only to be greeted with an electric shock. Eventually, the healthy mice and the SAM treated mice learned to associate the aversive shock with the dark chamber. In contrast, the Alzheimer’s mice were not able to make that association as successfully. “The Alzheimer’s mice forget that they’re going to get shocked and jump through the hole much quicker than the healthy mice type and the mice treated with SAM,” Salazar said.
Strittmatter, Salzaar, and other lab members are currently at work determining the ideal dose for SAM and the longevity of the drug’s effects. If all goes well, Strittmatter hopes to take SAM to clinical trials. Designing an effective Alzheimer’s drug has been difficult, partially because there is still a lot about the disease that we still do not know. Perhaps the ability of SAM to specifically target only abnormal protein interactions without interfering with normal mechanisms in the brain will yield more promising results.
About the Author:
William is a sophomore Neuroscience major in Morse College. He is the copy editor for the Yale Scientific Magazine and works in Professor Forscher’s lab studying the cytoskeletal dynamics underlying neurodegenerative diseases.
The author would like to thank Professor Strittmatter and Santiago Salazar for their time, and for sharing their passion and dedication to their research.
Further Reading:
https://www.cell.com/cell-reports/abstract/S2211-1247(17)30820-3