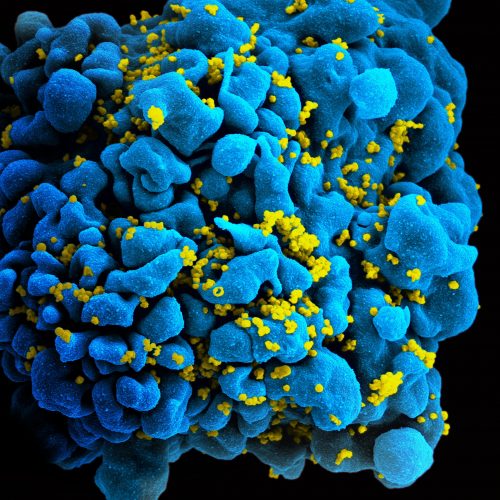
One of the most pressing problems today in the effort to eradicate HIV is latency. Infected T cells may harbor the virus but lie dormant for years, making up a latent reservoir that evades the drugs, which effectively kill only active cells replicating the virus. Researchers have recently discovered a new way to uncover cells harboring latent forms of the virus, opening the door to a new approach to extinguishing reservoirs of infected T cells inside a patient’s body.
Recently published in Nature Scientific Reports, the project was headed by Linda Fong, a graduate student in the laboratory of Kathryn Miller-Jensen, Associate Professor of Biomedical Engineering at Yale University. Her team studied five cell-signaling pathways in an attempt to distinguish infected cells from healthy ones. Signaling pathways are essential in multicellular organisms, since they facilitate how external and internal stimuli trigger changes in cells. These changes include events like releasing a hormone or expressing a gene. Before Fong’s team could study these pathways, however, they needed to reactivate the latently-infected T cells.
To do this, several classes of latency reversing agents (LRAs) were used to stimulate the cells. One type of LRA functions by opening up the cell’s chromatin, where the virus’s genetic information is found, to allow for the transcription and expression of the HIV genome; others are able to activate specific proteins leading to expression of the HIV genome. These agents are currently of great interest to HIV researchers looking to “activate-and-kill” the latent reservoir.
Once the T cells were treated with LRAs, researchers compared levels of kinase phosphorylation in infected cells and healthy ones. Kinases are enzymes that play an essential role in cell signaling pathways by transferring a phosphate from ATP, a molecule in which energy is stored, to another molecular substrate—usually a key protein in a cell signaling pathway—effectively activating or deactivating the protein. This transfer releases energy so that the signaling pathway can continue. The researchers realized that infected cells exhibit a significantly higher level of kinase phosphorylation than do healthy cells. Mathematical analyses further confirmed that the extent of variation in phosphorylation between infected and healthy cells was sufficient to differentiate them. This increased level of phosphorylation in infected cells indicates that the virus has managed to deregulate crucial cell processes, shedding light into one of the many ways the virus impacts the cells harboring it.
“You can imagine that if scores of scientists were working on this, you could find so many other pathways that are dysregulated,” Fong said. “That comes back to pathway engineering and the idea that you can get a cell to do what you want if you understand its circuitry.”
Previous research has compared latently-infected and healthy T cells in a state prior to reactivation by LRAs. These studies were unable to find an accurate, specific way to distinguish latently-infected from healthy cells.
These findings could have meaningful clinical implications, and Fong is working towards eventually conducting trials in HIV patients. For now, she has transitioned from testing healthy cells that are manually infected with HIV to working with cells extracted from the blood of HIV-positive patients. Ultimately, Fong and her team hope that their work will enable more selective and specific eradication strategies that target only infected T cells while leaving the healthy onces intact in patients with HIV.
References
[1] “Systems analysis of latent HIV reversal reveals altered stress kinase signaling and increased cell death in infected T cells” – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5701066/
[2] “Yale researchers root out latent HIV viruses” – https://yaledailynews.com/blog/2017/12/07/yale-researchers-root-out-latent-hiv-viruses/
[3] Interview with Linda E. Fong, Department of Biomedical Engineering, Yale University on February 2nd, 2018.