A Potential Treatment for Colorectal Cancers
Imagine two twins who, though identical in every respect from height to facial features, differ in a single gene. One twin has it, the other does not. Yet, the cascade effect is staggering—just one missing gene results in a viciously unregulated cell growth. Left uncontrolled, the cell cycle repeats on loop. Cells accumulate in the body, eventually becoming devastating, cancerous tumors. How could things have gone so wrong?
Researchers at Yale University, overseen by Professor of Pharmacology Dianqing Wu, discovered a new role of the protein called Dickkopf-related protein 2 (DKK2) that is overexpressed when cells lack a certain regulatory gene called adenomatosis polyposis coli (APC). Without the APC gene, DKK2 levels increase, promoting growth of cancerous cells, eventually forming tumors. Suppression of DKK2 using a novel antibody shows promising results in promoting activity of tumor-killing immune cells. Moreover, their research, published in Nature Medicine, demonstrates how blocking the function of DKK2 encourages the host’s own immune system to fight against cancer cells. Taken together, their results present promising implications for improving the efficacy of immunotherapy treatments for those with colorectal cancer.
A background on colorectal cancers
Over 80 percent of colorectal cancers are caused by a mutation in APC, a gene which is responsible for regulating a cell-signaling and growth pathway called the Wnt/β-catenin pathway. iIn past research, this pathway has been shown to affect blood glucose levels and bone mass as well as play a role in embryonic development and gene expression. Without the APC gene, the Wnt/β-catenin cell signaling pathway is hyperactive, resulting in overproduction of cells and eventual tumor formation.
Previous research has shown that in normal cells, DKK2 interferes with the Wnt/β-catenin pathway, preventing cell signals from being passed along to continue cell division. Therefore, it seems intuitive that a decrease in DKK2 would increase the activity of the Wnt/β-catenin pathway, which would subsequently increase cell proliferation and increase the number of tumors, right? Not quite—the story is much more complicated.
A blockade to the study
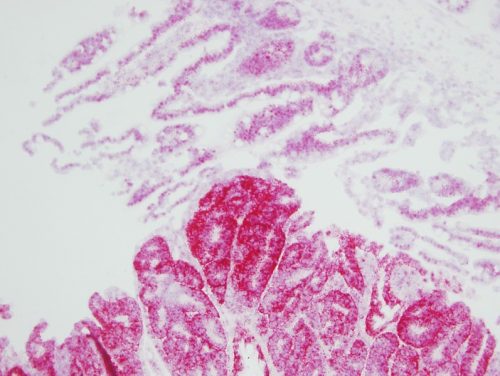
By analyzing gene expression databases, the researchers noticed that DKK2 expression is significantly higher in colon cancer samples, particularly in those likely harboring the APC mutations, than in normal ones. The researchers went on to determine whether DKK2 expression differed between hosts with the APC gene and those without. In order to study this, researchers used a cancerous mouse model with the APC gene suppressed through genetic engineering techniques, which models the human condition. The researchers found a significantly higher expression of DKK2 in mice lacking the APC gene. Even more, samples of human colon cancer cells indicated a correlation between increased expression of DKK2 with higher rates of normal cell death. This left the researchers wondering about the role of this protein—as well as whether they could regulate overexpressed DKK2.
One way to determine the role of DKK2 is to block the function of the protein and observe the resulting effect. The researchers used two means to create the DKK2 blockade: a genetic approach by which the DKK2 gene is disrupted in mice and the pharmacological approach by which an antibody, termed 5F8, was generated to neutralize DKK2 activity. Following DKK2 blockade via either the genetic approach or treatment with 5F8 antibody, they found lower occurrences of tumor formation in the intestines of mice and increased survival of these tumor-bearing mice. This means suppression of DKK2 is attributed to better health outcomes. Furthermore, these conclusions support DKK2’s role in tumor progression, where a larger amount of the protein significantly increased the severity of tumors formed.
Getting to the bottom of it
Having deduced the role of DKK2 on increasing tumor formation, the researchers’ next goal was to uncover the exact mechanism of their protein’s function. Specifically, the researchers were interested in exploring the relationship between the DKK2 blockade with natural killing (NK) and CD8+ cells. These immune cells are crucial for targeting and killing cancerous cells. What would happen if these immune cells were not present in APC-lacking cells treated with the DKK2 blockade? To test this, the researchers treated the mice with antibodies specific to both NK and CD8+ cells, depleting these cells. They found that DKK2 antibody treatment was no longer effective—the blockade could not suppress tumors without these immune cells.
From these results, the researchers concluded DKK2 plays a role in controlling the immune system’s ability to monitor the tumor environment. Of interest to Wu and his team was investigating the mechanism in which DKK2 influenced these immune cells. To determine whether the mechanism could be attributed to cell signals sent through the nWnt/β-catenin pathway, the researchers then treated cancer cells with a protein known to activate the pathway. However, they found no effect on suppression of NK cells, suggesting that DKK2 was not inhibiting immune cells through Wnt/β-cateninn. Moreover, they arrived at a surprising conclusion: DKK2 is acting independently of the Wnt/β-catenin pathway and suppresses the activity of interleukin-15, an important cytokine for NK and CD8 T cell functions via a previously unknown mechanism. Taken together, the researchers’ discovery has implications for future treatment methods for colorectal cancer.
A promising potential for cancer treatment
Current immunotherapy treatments are effective for a subset of colorectal cancers, termed microsatellite instable (MSI), but not for the subset largely caused by mutations in the APC gene, termed microsatellite stable (MSS). Using treatment of 5F8 in mouse models, the researchers found the antibody was effective not only in MSI, but also MSS, leaving the researchers to ponder the effect of combination treatment of antibody with current immunotherapy treatments.
To determine how treatment with the 5F8 antibody affects health outcomes when used in conjunction with a current immunotherapy treatment for both MSI and MSS colorectal cancers, the researchers then treated a mouse model with both drugs. The current immunotherapy treatment inhibits tumor cells from evading the immune system in MSI colorectal cancers, but not MSS. “We wanted to see whether our mouse models would show higher survival rates with combination treatment,” Wu said. The results were promising—treatment of the current immunotherapy drug together with 5F8 antibody promoted greater MSS tumor suppression than the antibody alone.
Yet, these results do more than overturn what was originally thought to be the role of DDK2. For starters, the team’s antibody successfully blocks the function of DKK2, thereby suggesting the efficacy of this antibody in reducing tumor formation. The second significant finding from their study is that this antibody serves as a potential therapeutic treatment for those with colorectal cancers. While current immunotherapy treatments help immune cells called T cells identify and attack cancerous cells, they are often less successful in colorectal cancers. Therefore, the 5F8 antibody may be used in conjunction with current immunotherapy drugs to further suppress tumors. “The combination of the two [drugs] will show a better, synergistic outcome,” Wu said.
There are still unanswered questions and drawbacks to address. For instance, DKK2 is not the only protein that causes tumor immune evasion. Other proteins and their mechanisms of action remain to be discovered. In addition, the team’s research was done on mouse models, and their results may not be aligned with that of human models.
However, the researchers’ discoveries contextualize DKK2’s malignant role in tumor formation. Pushing forward, Wu states the necessity of further tests in human models before the antibody can be considered for cancer treatment. The research team has licensed this intellectual property to a biotechnology company that will test the antibody further. If all goes well, there could be another drug on the market to treat colorectal cancer and related melanomas. “Our next step is to see if DKK2 blockade can really show efficacy in treating human colorectal cancers. We are very hopeful,” Wu said.