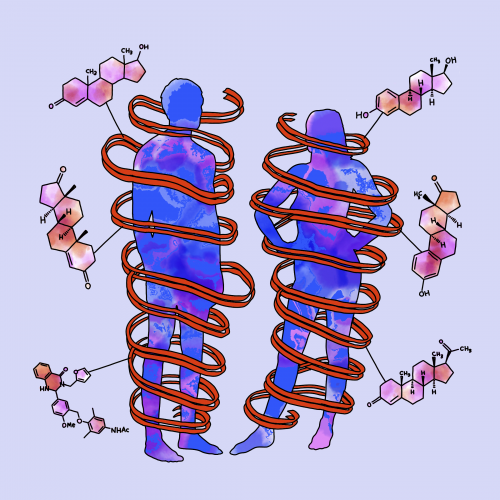
Art courtesy of Anasthasia Shilov.
Until almost thirty years ago, half the United States population was excluded from scientific research. It was not until 1993 that the NIH Revitalization Act required researchers to include women in scientific studies. Male and female physiological systems are inarguably different and consequentially express separate immune responses. To further explore this sex-based distinction, Nina Stachenfeld, a professor and researcher at Yale School of Medicine (YSM), has helped the Federation of American Societies for Experimental Biology Journal (FASEB) compile a series of reviews, “Sex as a Variable in Human Research: A Systems Approach.” This series recognizes sex differences in physiological responses to diseases like addiction and high blood pressure as well as today’s changing concept of gender identity and how this affects research.
In the past, many scientists excluded women from studies, believing that physiological responses were identical between sexes. Many later complained that women presented difficulties in hormonal regulation. “Estrogen, for example, has an impact on blood pressure regulation. [So,] if we’re studying women, we want to ensure that we’re controlling for estrogen levels and being cognizant of when we might test them in the [menstrual] cycle,” Stachenfeld explained. Regulating these factors may seem painstaking, but Stachenfeld counters that these aspects can be easily screened for and monitored. “Physiologists who do these kinds of studies control for [fickle factors] all the time, and they’re not easy to control for, but we do it,” asserted Stachenfeld. Scientists are already precisely regulating factors like environmental temperature, so including women in research may only require additional preliminary surveys regarding menstrual cycle timing, contraceptives, and pregnancy possibility. Ultimately, hormonal regulation in females is a minute inconvenience when compared to the necessity of including women in research.
Stachenfeld explained that once scientists were forced to conduct research on women, they began noticing big differences in female systemic regulation and treatment response. “It could [even] be as simple as dosages being too high, given that women are generally smaller than men,” Stachenfeld described, referring to blood pressure medication. Including women in research has elucidated many simple differences, profoundly affecting treatment development and clinical practice. In her own research, Stachenfeld focuses on cardiovascular disease, which often presents incongruously between sexes. “When a woman comes to the doctor and describes certain symptoms, the doctor can recognize that she’s maybe having a mild heart attack; in the past, the doctor might have thought that it was just indigestion,” Stachenfeld notes. These distinctions are invaluable to clinical care and were recognized only when women began to be included in medical research.
In August, a study by Yale researchers highlighted how men and women express different physiological responses to COVID-19, with men exhibiting weaker immune responses (see pg. 16 of the print issue). By including women in studies, researchers began recognizing that these sex differences actually exist in physiological responses and could even offer insight into the disease’s underlying mechanism. These understandings may lead to new developments for researchers working in drug discovery and vaccine development, which is especially important in light of the COVID-19 pandemic.
Previously, many researchers believed that all mechanistic work had to be done in animals, because humans posed numerous ethical concerns. However, “scientists have come up with incredibly creative ways to examine humans and their responses,” Stachenfeld explained.
Animals remain crucial to research, but they are not the same as humans. “Eventually, we do have to take that step [to reach our ultimate goal] to improve and impact human health,” Stachenfeld pointed out. As scientists urgently perform trials and research for COVID-19, they must also focus on the sex-specific physiological responses in humans and the subsequent implications.
When considering the effects of the COVID-19 pandemic, Stachenfeld has echoed Yale School of Medicine Dean Nancy J. Brown’s sentiment that the pandemic offers a unique opportunity to create structural modifications at Yale. Stachenfeld believes that the pandemic is motivating necessary changes in YSM related to both COVID-19 and gender equality. Additionally, Stachenfeld co-chairs the Committee on the Status of Women in Medicine (SWIM), which advocates for improvements in YSM’s structure surrounding sexual harassment and gender equity policies as well as the perception of women and their role in medical academia.
Celebrating the fiftieth anniversary of women at Yale, we must recognize that our differences underlie and enrich our unity. Women and men have varied perspectives, but these diverse experiences supplement the entire community with a more comprehensive mindset. Similarly, female and male physiological systems are distinct; recognizing these sex differences in research contributes to advancements in not only women’s health but also treatment development, which benefits all sexes.
Citations:
Harrison, R. (2020, September 04). Sex differences in COVID-19 immune responses affect patient outcomes. Retrieved September 26, 2020, from https://news.yale.edu/2020/08/26/sex-differences-covid-19-immune-responses-affect-patient-outcomes
Stachenfeld, N. (2020, June 30). Introducing a special series, sex as a variable in human research: A systems approach. Retrieved September 26, 2020, from https://faseb.onlinelibrary.wiley.com/doi/full/10.1096/fj.202001425