Every year, millions of patients recover from life-threatening surgeries and other medical procedures, only to get a secondary infection caused by the presence of bacterial, fungal, or viral particles on medical implants. In fact, the Centers for Disease Control (CDC) estimates that healthcare-associated infections account for an estimated 1.7 million infections and 99,000 associated deaths each year in the United States alone. Medical implants such as catheters, pacemakers, and prosthetic joints act as ideal habitats for biofilms—bacterial colonies that aggregate on smooth surfaces and remain highly resistant to treatment with antibiotics.
In the past, the only methods for treatment involved surgical removal of the implant or degradation of the biofilm using enzymes, which often had toxic effects on the human body. Researchers at Pulmobiotics, a spinoff company from the Center of Genomic Regulation in Spain, have recently developed a state-of-the-art technique to solve this problem: “living medicine,” or the introduction of genetically engineered bacteria to fight the dangerous pathogens within the body.
In this technique, researchers decide on a “good bacterium” to use, then remove specific genes to eliminate the infectious or disease-causing capability of the bacterium. They then equip the bacteria with an engineered genetic platform designed to secrete antibiofilm and bactericidal enzymes—giving the bacteria the ability to disintegrate or “fight” infectious biofilms.
Maria Lluch Senar, a biotechnologist who formerly worked at the Center for Genomic Regulation before founding Pulmobiotics with her research partner Luis Serrano, has been working with the bacterium Mycoplasma pneumoniae for over ten years in an attempt to characterize its genome. Ultimately, the researchers sought to create a bacterial chassis, a genetic framework that could house and support exogenous DNA without interfering with the bacterium’s functional purpose: targeting ventilator-associated pneumonia.
With a mortality rate of ten to fourteen percent, ventilator-associated infection is caused by pathogenic bacteria like Staphylococcus aureus, which “grow in thick layers that are very difficult to target by using conventional antibiotics because [the antibiotics] cannot cross [the bacterial] barrier,” Senar said.
Thus, the lab aimed to engineer a bacterium that could fight against biofilm infections: removing the pathogenic factors of M. pneumoniae DNA while concurrently adding synthetic promoters and sequences designed to destruct S. aureus biofilms in the lungs.
The researchers chose to use M. pneumoniae for their microbial chassis due to several favorable biological characteristics. The bacterium, for example, had known activity in lungs. “When you want to engineer a live biotherapeutic, it is important to look for bacteria that is naturally present, or already colonizing, the target organ,” Senar said. M. pneumoniae also had a genetic advantage: “The strain has a unique genetic code that prevents gene transfer,” Senar said. Moreover, M. pneumoniae’s slow division allowed for an expanded production time scale in the lab and provided additional control over the bacteria’s replication rate in vivo. Thus, if there was a major problem with the delivery system of the chassis, it was easier to contain the spread of bacterial growth and remove the bacteria from the patient’s lungs.
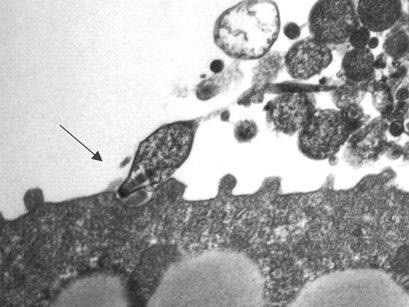
However, the biggest advantage of M. pneumoniae was its lack of a cell wall. The immune system’s pathogen recognition mechanisms often target bacterial cell walls; thus, this feature of M. pneumoniae would allow it to escape immune recognition, preventing host elimination of the microbial chassis. This also allows for a combined treatment approach: after the bacterial chassis secretes biofilm-dispersing agents, antibiotics and bacteriolytic enzymes can be co-administered to attack the cell wall of S. aureus without damaging M. pneumoniae.
The researchers delivered the biofilm-fighting genes to M. pneumoniae with plasmids, circular pieces of DNA that can be transferred from cell to cell. They assembled the plasmids from DNA fragments of genes of interest using the Gibson method, a molecular cloning technique. Of interest, the researchers delivered genes that drove continuous, localized production of dispersin B, a hydrolytic enzyme that breaks down S. aureus bacterial cells, to provide long-term disruption of the biofilms. After genetically engineering their M. pneumoniae, the researchers tested their chassis in mice models to verify its safety and efficacy.
The research team is also looking beyond S. aureus biofilms. Due to the natural ability of M. pneumoniae to colonize the respiratory tract, bacterial therapies hold important future potential in many medical therapies. “The 21st century is becoming the century of synthetic biology,” said Senar, highlighting genetic engineering’s increasing potential to create novel treatments for a wide range of diseases, from cancer to chronic obstructive pulmonary disease.