For a soldier returning from combat or a cancer survivor, the battle is not over even after recovery. These people are prone to severe, irreversible muscle loss, whether caused by a deep bullet wound or multiple rounds of chemotherapy. Their condition, called volumetric muscle loss (VML), is a daily struggle. Patients with VML lose the mobility of their limbs, which makes simple actions like walking, grasping, or even standing monumental challenges. To make matters worse, it is currently impossible to fully recover from VML. VML is difficult to treat because the regenerative capacity of muscles is limited. Once skeletal muscle is damaged, it often cannot regrow, especially when the extracellular matrix (ECM)—the structural support for cells and tissues that helps orchestrate growth—is lost. In these cases, growing muscle is like trying to build a house without a frame. This means that for the rest of their lives, most patients have no choice but to live with the stark reality of VML.
According to their paper published in Matrix Biology, a student team led by Themis Kyriakides, a professor of pathology and biomedical engineering at Yale, has found a potential cure. They engineered an innovative hydrogel that mimics the ECM’s role in building muscle. The hydrogel works by encouraging the body’s own cells to kickstart the process of creating new muscle tissue. The hydrogel offers a matrix for muscle cells to latch onto and begin the healing process, acting as a temporary foundation. Essentially, they’re providing the frame upon which the body can build a house.
This hydrogel is carefully constructed through a complex procedure. First, skeletal muscle tissue is subject to decellularization, which means stripping away the muscle cells to leave behind the ECM. Next, enzymes digest the ECM to form a solution, which can then be manipulated into a hydrogel. Through this process, the team was able to preserve the structure and composition of natural ECM in their hydrogel. However, there was one key difference—their hydrogel lacked a protein called thrombospondin (TSP-2). TSP-2 is normally found in muscle tissue and can hinder the regeneration process. The absence of TSP-2 slightly alters the flexibility of ECM, allowing cells to enter damaged tissue more easily. This hydrogel promotes blood vessel and nerve formation, making it highly effective for muscle regeneration.
Kyriakides’s hydrogel has the potential to not only help patients with VML cope with their condition but also fully restore muscle function. This breakthrough paves the way for a return to normalcy for patients with VML, who have often already sacrificed and suffered immensely. However, the clinical adoption of the hydrogel will require several years of rigorous testing and regulatory scrutiny. “The immediate plan is to show the efficiency and efficacy in large animal models before moving to human trials,” Kyriakides said. Furthermore, using the hydrogel alone will not lead to a full functional recovery—patients will still have to go through months of rehabilitation.
Even beyond treating VML, the hydrogel has broad applications in the world of regenerative medicine. It could be adapted for a variety of conditions, aiding skin regeneration after a severe burn or enhancing tissue repair in muscular dystrophies. With clinical trials on the horizon, this hydrogel could signal a new era for people with previously incurable muscle injuries—one where they may no longer have to face the pain of their conditions in their daily lives.
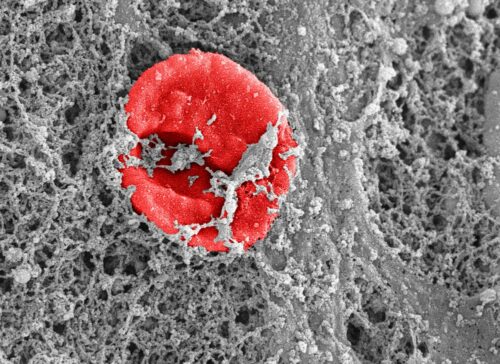
Image courtesy of Flickr.