Endometriosis, a chronic inflammatory condition, affects roughly ten percent of reproductive-age women worldwide. Characterized by tissue and lesion growth outside of the uterus, it is a debilitating disorder with limited treatment options and potentially permanent side effects. “Available drugs for endometriosis are very suppressive, […] stopping the ovaries from producing hormones,” explained Yingqun Huang, professor of reproductive sciences at the Yale School of Medicine and one of the study’s senior authors. “Most endometriosis cases are in reproductive-aged women, so you shouldn’t use hormone-repressive treatments long-term.”
In a recent study, researchers at the Yale School of Medicine co-led by Huang have discovered a promising new approach to treating endometriosis by targeting specific immune cells that drive its progression. The study focuses on a particular group of white blood cells, known as disease-associated macrophages (DAMs), which become dysfunctional in endometriosis. These DAMs overexpress the TET3 gene, fueling inflammation instead of resolving it. This inflammation, in turn, worsens endometriosis symptoms, perpetuating the cycle of pain and complications. Huang believes that blocking the activity of TET3 in these macrophages could interrupt this cycle and halt disease progression.
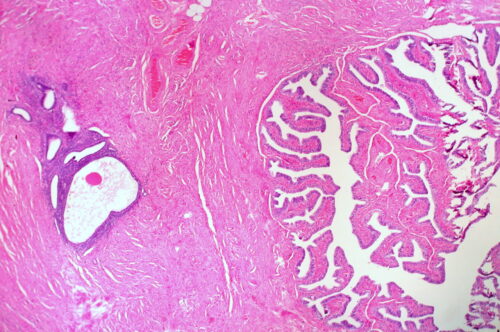
Enter Bobcat339, a synthetic compound the team tested for its ability to degrade TET3 in these disease-fueling macrophages. By activating a protein that breaks down TET3, Bobcat339 effectively blocks inflammatory activity. In mouse models, the compound significantly reduced inflammation and lesions associated with endometriosis. “What we’re trying to develop with TET3 is a drug that is more specific, targeting the root cause of endometriosis […] and that can be used long-term,” Huang said.
This promise of a more precise, less invasive treatment is part of a broader shift in how doctors understand endometriosis. “For years, doctors thought the only way to diagnose endometriosis was through surgery,” said Hugh Taylor ’83, a co-author of the study and Yale chair of obstetrics, gynecology, and reproductive sciences. “But now, we’re finally understanding how the immune system is malfunctioning in endometriosis, which is largely what causes the pain and the damage.”
Taylor’s career in women’s health has been driven by what he sees as major gaps in care for diseases like endometriosis. “Endometriosis patients were often told that periods are supposed to hurt and to ignore it—they’re dismissed by friends, family, even doctors,” Taylor said. “It’s an average of about ten years delay from the time someone has classic symptoms until the time it gets diagnosed, the two thirds of them, roughly, being misdiagnosed.”
Taylor emphasized that endometriosis impacts far more than just the pelvic area. Research now shows that it can lead to systemic issues like bowel irritation and even neurological symptoms such as depression and anxiety, which are typically treated as individual disorders. “Just look at the big picture and say, this is just endometriosis,” he explained. “Let’s try treating that first.”
Looking ahead, the team plans to explore TET3’s role even further, aiming to understand how it drives dysfunction in macrophages and how selectively eradicating these macrophages could reduce inflammation without harming the immune system. Huang and Taylor are optimistic that, with further study, Bobcat339—and other similar compounds—could offer new treatment options not only for endometriosis but potentially for other inflammatory diseases where TET3-overexpressing macrophages are involved. Ultimately, by focusing on the root causes of inflammation in endometriosis, this research signals a significant shift in the way endometriosis is approached. “We’re trying to really understand the pathophysiology, the biology, to come up with tomorrow’s cures,” Taylor said.