Art by Alondra Moreno Santana
Neither Kaiyue Ma GSAS ’23 nor Monkol Lek ever imagined they would work in genetics—Ma was an aspiring evolutionary biologist and Lek was an IBM engineer. But now as researchers at the Yale School of Medicine, the duo recently announced a new platform for genetic assays with the potential to improve diagnoses for those suffering from rare diseases.
The research has personal meaning for Lek, who decades ago developed a rare neuromuscular disease and struggled to find a diagnosis. From his insight into the patient experience, he decided to go back to school and research diseases like his. According to Ma and Lek, rare disease research is not profitable, and by definition, only directly impacts a few people. However, its effects ripple—spreading hope through the lives of their families, friends, and communities.
Last year, Ma, Lek, and their team developed a framework for accessible, cheap, and scalable genetic assays to investigate a group of rare genetic diseases. They recently published their work in Cell. Ma, the first author of the study, wanted a catchy name for this framework, something that he could actually picture scientists remembering, so he called it SMuRF, a name that encapsulates its small but mighty characteristics. SMuRF, which stands for “saturation mutagenesis-reinforced assays,” was developed as part of Ma’s PhD thesis.
Overcoming Obstacles
Current methods of rare disease diagnosis are incredibly resource-intensive, sapping patients’ time and money during an already stressful period in their lives. Ma explained that there are two main obstacles for rare disease patients. The first is to get an accurate diagnosis, which itself could take years. The second obstacle is to discover an effective treatment. SMuRF targets the first obstacle, improving clinicians’ ability to connect variations in genes to physical consequences in the body.
“We only know the genetic cause in about fifty percent of the cases,” Ma said. “Why is that? One of the reasons why is we haven’t discovered all the genes associated with the disease, and the other reason why is we don’t understand the different kinds of variants or DNA changes that we find in genes that associate with disease.”
Thanks to years of advancements in the field, geneticists can determine an individual’s genetic makeup relatively easily. The challenge is in interpreting the dizzying amount of data. Sorting through every change in the genome to deduce what makes patients sick or not involves taxing experiments with specialized reagents or even robotics. Previous methods may also rely on large numbers of genomes, which on the whole can take enormous amounts of time and resources to sequence and analyze. Instead, SMuRF employs a technique called deep mutational scanning (DMS) that can efficiently assess genetic mutations at a large-scale. DMS generates a collection of mutants, individually tests each variation, and compares which variants affect protein function.
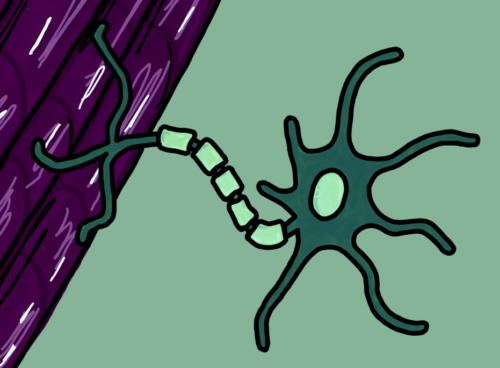
The team chose to first study dystroglycanopathies, a group of disorders that lead to muscular dystrophy, or degeneration of the muscles. Dystroglycanopathies are the result of mutations in proteins that serve like muscular glue, binding muscle cells to a network of proteins and other molecules called the cytoskeleton. Without this glue, the entire structure of muscular tissue begins to fall apart. Since the proteins related to dystroglycanopathies are known, the team utilized DMS to analyze every possible single-nucleotide variant of the two enzyme-coding genes involved. By delivering the created variants into the cells, they were able to analyze how well the enzyme functioned.
Essentially, SMuRF allows scientists to examine variants one by one, observing how tiny individual tweaks can create downstream consequences. Much like bricks in a game of Jenga, some variants are unimportant, while others are key to understanding the foundations of diseases. Though the study only tested SMuRF on dystroglycanopathies, the technique has the potential applications for other diseases because it is flexible and more cost-effective than previous experiments.
Time is Money is Muscle
Ma and Lek hope that SMuRF can be incorporated in clinical research labs across the globe, helping to shorten patient diagnosis time at a fraction of the cost. As a patient himself, Lek is very adamant that SMuRF and other rare disease assays should be affordable. He shared that when he first moved to Sydney before his time at IBM, he had nothing but the clothes on his back, and struggled to pay for basic needs, much less medical expenses. Because of this experience, Lek viscerally understands the need for affordable healthcare options.
Additionally, Ma and Lek hope that SMuRF will reduce the loss of another resource for patients: time. In the practice of rare disease therapy, a common saying is that “time is muscle.” Many patients with dystrophic muscular diseases are in a frantic race against the clock, struggling to find treatment before they lose control of their bodies. In some cases, the disease wins out before the patient can even be diagnosed. Since SMuRF is faster than other diagnosis tools, Ma and Lek hope that it will save time, muscle, and lives.
From Testing to Therapy
Though SMuRF might allow physicians to identify the genetic origins of diseases, that is only half of the battle. What is the importance of a diagnosis if there is no treatment?
Lek explained that part of his motivation to come to Yale was the dismay he felt when he had to deliver unactionable bad news. “I also wanted to work on therapy,” Lek said. “So the impact I want to make there is to actually create gene therapies that actually go into clinics.”
Similar to Lek, Ma wants to work to find treatment options, and since his PhD, Ma has transitioned into the field of evolution. “For those patients with advanced conditions, even though you can do gene therapies for them, it can only stop the further deterioration of the disease, it cannot restore the muscle tissue. It cannot repair the damage,” he explained. In his future research in evolutionary medicine, he strives to advance the technology of muscle repair.
In the future, Lek and Ma hope that their work will transition from labs to hospitals and improve the lives of undiagnosed patients by minimizing the length and financial strain of the diagnosis period.
“We need to work with real patients and patients’ families,” Ma said. Although they took winding and unconventional paths to genetic research, Ma and Lek’s problem-solving approach now has the potential to make incredible real-world impact, offering hope to individuals and families who have long been underserved in medicine.