When you are sick, do you ever lose your appetite? Your favorite meal suddenly seems less exciting, and you can’t taste the difference between cookies and cardboard. It turns out, there may be an evolutionary reason for this. Researchers at the Yale School of Medicine, in collaboration with the University of Texas Southwestern, have explored this phenomenon and recently provided exciting insight regarding the connection between host metabolism and how it can influence disease tolerance in cerebral malaria, which is caused by parasitic infection.
Linking metabolism and infection
At first, it seems counterintuitive that you would lose your appetite when you are sick—wouldn’t it make sense to eat more so that your body has the nutrients and energy to fight off an infection? However, there is more to the picture than this. “It turns out that animals from worms to flies to mice to humans lose their appetite when they get a serious infection,” explains Andrew Wang, a rheumatologist at the Yale University School of Medicine and lead author of this paper. “This has been particularly confusing because dealing with infection is generally thought to be a hypermetabolic state. So, why when you need more metabolic fuels would you stop consuming them?” Wang said. A hypermetabolic state refers to an increase in one’s metabolic rate, including increased energy production. There has been a historical hypothesis that one could instead “starve” a pathogen to cure an infection, which may be related to one’s loss of appetite. Because this idea had not been well studied before, his team sought to understand if this was connected to appetite loss. “These observations and this very basic problem was the conceptual backdrop which inspired our recent work,” said Wang.
Additionally, in 2016 Wong and collaborators found that appetite has an effect on the metabolic environment for fighting particular infections. For example, a bacterial infection may be best counteracted with a “fasting” state of low energy consumption, while a viral infection may require a “fed” state of high energy consumption to overcome. In either case, there was no difference in how strong one’s immune response was, including how well it killed the pathogen. However, there was a difference in how well one could tolerate the infection. This finding then inspired the researchers to look at what kind of metabolism was needed to tolerate a parasitic infection, and thus, motivated their recent work with cerebral malaria.
Disease tolerance in cerebral malaria
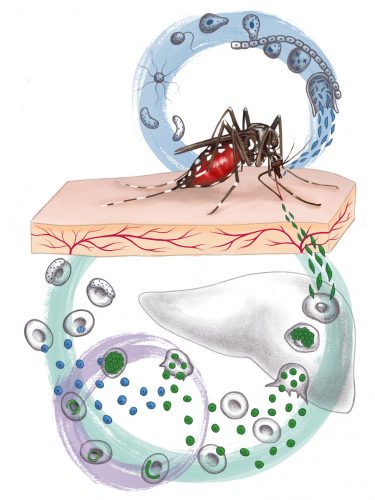
In their most recent paper, the researchers explored the hypothesis that an organism’s metabolism is important in responding to a given type of infection, with a particular focus on malaria, a disease caused by the parasite Plasmodium falciparum. Malaria is prevalent in impoverished nations, killing more than one million people per year, especially children under the age of five years. This investigation focused on cerebral malaria because it affects the brain, where metabolism is crucial for stress adaptation pathways that preserve brain function. In this study, mouse models of cerebral malaria were used to investigate the effect of glucose metabolism on disease progression.
Specifically, the researchers examined glycolysis, a critical process required for energy extraction from glucose. To determine what happens in mice with cerebral malaria, the researchers used 2-deoxy glucose (2DG), an analog of glucose that competes for an enzyme that transforms glucose into the next metabolic intermediate in glycolysis, in order to inhibit glycolysis in the mouse. This was done to directly assess the function of glucose in cerebral malaria.
When glycolysis was inhibited in mice with cerebral malaria using 2DG, the researchers found that mice lived longer by more than ten days and that the clinical signs of the disease were fully suppressed. However, this was insufficient to cure the mice because later complications of malaria arose over time, specifically the persistent presence of the parasite and severe anemia. “The Plasmodium parasite spends much of its life cycle in red blood cells and lyses them as it divides, causing anemia. The 2DG can support a mouse beyond cerebral malaria, but without antibiotic treatment, the mouse cannot clear Plasmodium and it eventually causes enough anemia to kill the animal,” said Wang.
2DG mediates disease tolerance
Another key finding of this study was that 2DG treatment did not affect the degree of pathogen burden in the brains of the mice, meaning that the number of parasites found in the 2DG-treated mouse brains were comparable to control mouse. This suggested that the function of 2DG is not to control pathogen load in order to protect mice from cerebral malaria.
Additionally, 2DG treatment did not impact cerebral edema of neuroinflammation. Cerebral edema causes swelling of the brain due to fluid retention, and is known to occur when the permeability of the blood-brain barrier (BBB) is disrupted by cerebral malaria. The researchers were interested in observing potential differences in neuroinflammation because this had previously been implicated in directing the development of this disease. Further, neuroinflammation was related to cerebral edema because increased permeability of the BBB is thought to be caused by inflammatory processes. For both cerebral edema and neuroinflammation, no differences were observed between 2DG-treated and control mice. These observations indicated that 2DG did not make mice succumb to hallmarks of cerebral malaria itself. Thus, 2DG must be acting through a different mechanism to protect against cerebral malaria.
The researchers next tested the hypothesis that 2DG acted on hemostatic parameters. Hemostasis, the cessation of bleeding, was relevant to this investigation because factors related to hemostasis, such as disruption of vascular blood flow and microthrombi, or blood clots, are also signs of cerebral malaria and proximally cause brain dysfunction and, ultimately, death. To see whether 2DG was affecting hemostasis, brain sections of both 2DG-treated and control mice were compared. They found that there were far fewer microthrombi in the brains of 2DG-treated mice, and in following experiments, that blood coagulation throughout the body was also affected because the strength of blood clots in 2DG-treated mice was weaker. These two major findings suggested that coagulopathy, the blood’s ability to form clots, is greatly impacted by glucose metabolism in mice with cerebral malaria. By inhibiting glycolysis, 2DG protected the diseased mice by enhancing its tolerance to the disease, specifically through decreasing the strength of malaria-induced blood clots and thus decreasing the hemostatic problems that malaria causes.
Metabolism and infectious diseases
This research provides much excitement for future treatment of infectious diseases, including, but certainly not limited to, cerebral malaria. Current treatments for cerebral malaria, such as antimalarials, are still not completely effective. “Part of this has to do with the fact that, like with many inflammatory syndromes caused by infection, what often causes pathology is not the pathogen itself but the inflammation caused by our immune response to the infection, which in the case of malaria causes microvascular changes, clots and bleeds,” explained Wang. In this context, 2DG may be useful because it works differently than antibiotics.
2DG as a therapeutic is currently in clinical trials for cancer because it is known that cancer cells tend to use glucose via anaerobic glycolysis over more energy-efficient production methods, such as oxidative phosphorylation. This phenomenon is termed the Warburg effect. However, more thorough study of 2DG and its side effects is needed to assess its safety and efficacy.
The enthusiasm surrounding this research linking host metabolism with disease tolerance is growing. The concept of “targeting” one’s metabolism to alter the progression of an infectious disease is a novel and fascinating avenue to explore. “Most drugs in inflammatory diseases, either infectious or not, have focused on disease resistance. We think that equally important is to learn how cells and tissues tolerate physiological changes caused by inflammation,” said Wang. However, he also noted that much more work needs to be done in this field to ensure that the biological mechanisms are well understood. Furthermore, such work would then need to be translated from model organisms to humans.
“Understanding these cellular and tissue tolerance mechanisms, which is a very exciting new frontier, could lead to the development of novel therapeutics that could improve outcomes in many inflammatory diseases with great unmet need, like sepsis and cerebral malaria,” concluded Wang. Indeed, this frontier remains open for exploration. As the realm of inflammatory diseases is vast, from asthma to rheumatoid arthritis and beyond, the possibilities for new drug therapies seem endless.