Everyone generates cancerous cells. The human body is made up of more than a hundred million cells that may mutate during the process of division to grow uncontrollably—i.e. become cancerous. However, the human immune system has built-in mechanisms that detect and destroy cancerous cells before they can spread. Cancerous cells only becomes a threat when the immune system either fails to detect them or cannot keep up. An innovative branch of cancer therapy known as immunotherapy accelerates the natural immune response to destroy cancerous cells, avoiding the toxic side effects associated with traditional cancer treatment.
Because cancer cells are defined by their uncontrolled, rapid growth, standard chemotherapies target rapidly dividing cancerous cells but also kill rapidly dividing normal cells, such as those in the stomach lining and in hair follicles. The death of these normal cells leads to the short-term side effects associated with chemotherapy, such as nausea and hair loss. Chemotherapy can also cause neutropenia (low white blood cell count), rendering the body unable to fight off infection.
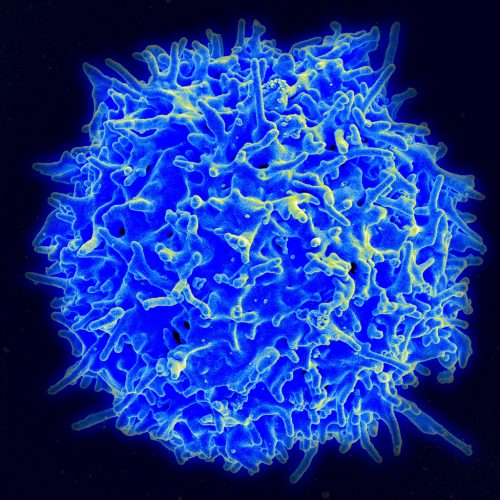
Instead of introducing toxic medication into the body, immunotherapy amplifies the adaptive immune response made up of B cells (produced in the bone marrow) and T cells (produced in the thymus). B cells recognize antigens displayed on the surface of foreign cells and secrete antibodies that mark them for destruction by T cells. Immunotherapy approaches include vaccinations that increase antigen display to mark cancerous cells for destruction, viruses that infect and kill tumor cells, and reprogramming T cells to recognize specific antigens displayed on the surface of cancer cells, which is known as chimeric antigen receptor (CAR) T-cell therapy.
In CAR T-cell therapy, a patient’s own T-cells are engineered to have a receptor protein that corresponds to a specific antigen on the surface of the target cancer cell. When these specially-engineered T cells are injected back into the patient, they bind to cancer cells and kill them. Simple in theory, this treatment remains imperfect. Large-scale T-cell activation leads to cytokine release syndrome, which has severe, flu-like symptoms. Neurotoxicity is an even more worrisome side effect. Additionally, it is necessary to determine an antigen that is specific to every cell of a particular cancer but not found on essential cells; otherwise, there is a risk of CAR T-cells killing the patient’s own cells, as in chemotherapy. Even if the correct antigen is found, not every patient responds positively to CAR T-cell therapy.
Since 2008, scientists have postulated that polyfunctionality (co-secretion of as many immune function proteins as possible) increases the quality, potency, and durability of CAR T-cell therapy. It is not entirely understood why polyfunctionality varies among CAR T cells, but it is likely that either the variable manufacturing process or differences in original T cells among patients is responsible. CAR T-cell therapy differs from conventional drugs because it is a personalized, living drug, resulting in polyfunctionality quality inconsistences that could not be detected prior to infusion until now.
IsoPlexis, a start-up company founded by Rong Fan, Associate Professor of Biomedical Engineering at Yale and Chief Scientific Advisor for IsoPlexis, has created a single-cell antibody barcode microdevice that measures levels of polyfunctionality, thus predicting the success of CAR T-cell therapy. A study from Kite Pharma and IsoPlexis examined anti-CD19 cells used to treat non-Hodkin’s lymphoma (NHL), a cancer of the lymphatic system that typically originates in B cell progenitors. Anti-CD19 CAR T-cells are engineered to bind to the protein CD19 found on the surface of all B cells, killing both B cells and NHL cells. Fortunately, B cells are considered non-essential, and it is possible to live without B cells if a patient receives antibody injections.
The study determined the polyfunctionality of anti-CD19 CAR T cells using IsoPlexis’s new technology and verified a positive correlation between polyfunctionality and NHL patient responses. Now, IsoPlexis’s technology may be used to assess the quality of CAR T-cells and the predicted patient response before injection, guiding scientists to create more effective CAR T cells. Fan’s lab is currently combining this technology with genome editing to create high-quality CAR T cells with high degrees of polyfunctionality, maximum efficacy, and minimized immunotoxicity.
“Our technology could become a standard test for quality control in all CAR-T or other immune cell therapies,” said Fan. “It may even find uses as a routine test to monitor patients over the course of treatment to ensure activated immune cells are doing their job and in the right way.”