You share 99.9 percent of your genetic material with the person sitting next to you. This genetic material, or DNA, encodes the proteins your body produces and, by extension, all of your traits. However, despite your genetic similarity, your neighbor and you may have drastically different responses to the same pharmaceutical compounds. While you may respond positively, they may not respond at all—or maybe even negatively. The question of what causes this diversity of reactions to pharmaceutical compounds has puzzled scientists for decades. Past research has focused on the 0.01 percent of DNA that is different and has attempted to link reactions to differences in the liver enzymes involved in the metabolism, or the breaking down, of pharmaceuticals. But what if the difference lies not in our genes but in the genes of bacteria living inside of us?
Last month, researchers in the Goodman lab at the Department of Microbial Pathogenesis at the Yale School of Medicine found that our gut bacteria are involved in more than just the metabolism of food. They identified an important role of the microbiota in drug metabolism, offering an explanation for the diversity of human drug responses.
What is the Microbiome?
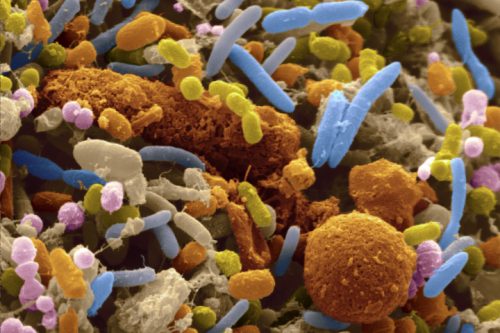
Despite the near-identical genetic composition among humans, the bacteria community that thrives inside us, also known as the microbiota, varies immensely. Hundreds of species of microbes totaling around 100 trillion cells live on our skin, in our intestinal tracts, in our mouths—all in harmony with our normal daily processes. “The microbiota can be thought of as the backpack of bacteria we pick up and bring with us through the journey of life,” explained Michael Zimmermann, co-lead author of the paper.
While we start off germ-free, we are immediately introduced to bacteria through the birth canal, the nurse at the
hospital, the pet at home, and everything else with which we interact. Although the microbiota eventually stabilizes around age three, factors such as what you eat and where you live continue to play a role in microbe abundance and diversity. The question of what is at the root of microbial differences between humans is an ongoing research topic. Nonetheless, the makeup of our microbiota is highly subjective to our living conditions.
In fact, human microbiota can be up to one hundred percent different with regards to what species exist and in what ratio. These microbes have genes of their own, which are known as the microbiome. A human’s microbiome is a hundred and fifty times the size of the human genome. The sheer amount of DNA presented a challenge to investigators researching the microbiome—that is, until the advent of next-generation gene sequencing.
It is important to note that most bacteria in the microbiome are not the disease-causing harmful type often associated with the name. They are crucial to the normal functioning of their host organism. For instance, we could not produce vitamin B12 without our gut flora. In this way, we are intimately linked to our microbiota, and this link may extend to how our bodies process drugs.
Microbiome and Drug Metabolism
When you take a drug orally, part of it is absorbed into the blood and broken down by the liver. The remaining amount travels through your digestive tract and remains in the intestine to be broken down by the bacteria there. With this in mind, the researchers decided to look for a known drug that elicits different responses in different individuals. They settled on brivudine (BRV), an antiviral drug used to treat shingles that acts by inhibiting viral replication. In some individuals, it can be broken down into the toxic product bromovinyluracil (BVU). To determine whether gut bacteria plays a role in the process, a preliminary experiment was performed in a test tube (in vitro) to test the effects of gut bacteria on BRV metabolism. The common gut bacteria Bacteroides thetaiotaomicron, which typically helps digest complex carbohydrates, was grown in the presence of BRV. It was found that the bacteria did produce BVU, implying that BVU production is at least partially due to the bacterial activity.
The activity of B. thetaiotaomicron was then examined in sterile mouse models. Some mice were infected with wild-type bacteria that breaks down BRV into BVU; another model was populated by mutant-type bacteria that does not break down BRV. The wild-type mice were found to have five times more BVU in their blood than the mutant mice, implying that a majority of BVU production was due to bacterial metabolism instead of host metabolism. Further examination with mathematical modeling showed that bacteria produced seventy percent of the toxin, while the host produced only produced thirty percent. Testing with the anti-anxiety drug clonazepam revealed a similar distribution: eighty-five percent bacterial production versus fifteen percent host production. Across a spectrum of drugs, the bacteria were more involved in the production of toxic byproducts than the host.
Overcoming Obstacles
Mathematical modeling helps scientists find what they do not understand about a process. As they test out different conditions in real life, scientists examine how their predictions in a mathematical model compare to reality. Divergence between predictions and reality indicates that there is some factor that is not accounted for in the model. “Mathematical modeling is a cycle: you go back and forth between observations and modeling. When the data doesn’t match, you make new models or add in a measurement to the observation,” said Maria Zimmermann-Kogadeeva, co-lead author of the paper.
When modeling the drug metabolism process in the mouse body, Zimmermann-Kogadeeva had to account for the final location of every single molecule of drug that went into the mouse. A system of differential equations was used to describe the drug as it moved from the blood to tissues to excretion. To determine how much drug was available to the bacteria to break down, the amount of drug metabolized by the host was subtracted from the original dosage. However, when applying the model to clonazepam—the anti-anxiety drug—their model failed to predict their observations. The bacteria in the mice were producing more toxic product than the amount of drug available to them—something which the model could not explain.
After numerous discussions together, the researchers determined that the process of metabolism is just as back and forth as the process of mathematical modeling. Clonazepam can be chemically modified in three different ways: aminoreduction (performed by both the liver and bacteria), hydroxylation (performed by only the liver), and glucuronidation and deglucuronidation (performed by bacteria following hydroxylation). When Zimmermann and Zimmermann-Kogadeeva further examined the chemical structure of the metabolized drug molecule in the gut, they saw evidence of previous hydroxylation. From this observation, they concluded that, after the mouse’s liver metabolized the drug into a chemically transformed product via hydroxylation, the gut bacteria could convert it back into the toxic product via glucuronidation. Thus, no drug product was lost to the host’s metabolism, as the model had previously predicted. The interactions of host metabolism and microbes are not one-directional; they are complicated back-and-forth cycles whose effects are difficult to isolate.
Manipulating the Microbiome
Knowing how gut bacteria contribute to drug metabolism allows us to personalize medicine based on an individual’s microbiome. “The microbiome could impact medicine from the very beginning of the process at drug development to the very end of the process at the level of the individual patient,” Zimmermann said.
Just as we use genetic screening to determine which drugs are most likely to respond favorably to a particular patient, we may one day do microbiome screening. We can also use models of drug metabolism by the microbiota to design better drugs that are resistant to metabolism by bacteria and cannot be converted into toxic byproducts by the microbiome. Most radically, we could use our knowledge of the microbiome to change it for the better. We could use antibiotics to eliminate bacteria like B. thetaiotaomicron that release toxic products, and probiotics or fecal transplants to repopulate good gut bacteria to a normal level. Even though the paper focuses on the bacteria that produce toxins, microbes are also crucial to keeping us healthy— they help with hormone production, the development of our immune system, the breakdown of chemicals, and the production of complex structures.
The microbiome has been overlooked for decades because of a focus on human genes instead of the genes of the bacteria inside of humans. By offering an explanation for the diversity of patient responses to therapeutics, and potentially to a wide variety of questions, this study reinforces the need to pay the same, if not more, attention to our microbiome. In such a new field, there is still so much unknown. Piece by piece, we add to our understanding and reverse misconceptions of the past. “The more we know about the microbiome, the more we can control it and make informed decisions about drug therapy and lifestyle,” Zimmermann-Kogadeeva said.