Image courtesy of Flickr.
Every year, nearly eight hundred thousand Americans experience a stroke, each with a possibility of brain damage or death. Following such brain injuries, the body attempts to repair the damaged tissue, beginning with neural stem cells (NSCs). Once signaled, NSCs proliferate and migrate as a cluster to the olfactory bulb in the brain to differentiate and repair damaged tissue. However, the mechanisms triggering NSC clustering were hidden in relative obscurity.
That was until a team of Yale researchers led by recent graduate Rita Matta and professor Anjelica Gonzalez in the Department of Biomedical Engineering decided to investigate how endothelial cells (ECs), which constantly exchange signals with NSCs because they line the blood vessels along which they move, may contribute to NSC clustering and migration.
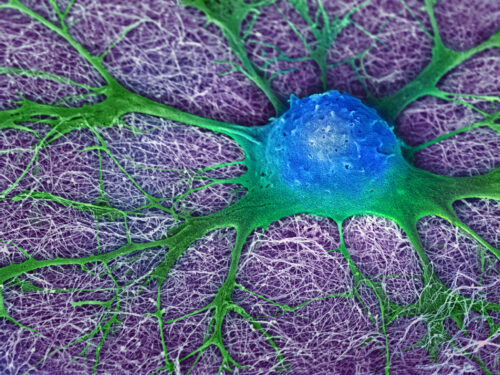
By studying cell cultures, the team established that ECs promote NSC clustering and migration. However, clustering itself must be actuated by something else. The culprits behind that were leader cells, special NSCs that sense the microenvironment and guide the cluster to areas of neural injury by extending cell arms. Their presence opened a new avenue for exploration.
In collaboration with professor Michael Murrell and post-doctoral associate Sulaiman Yousafzai Muhammad, migration and clustering were observed using multiple sophisticated engineered systems, including microfluidic chambers, traction force microscopy, and laser ablation. Ablation of the leader arm resulted in no migration of NSC clusters, even in the presence of ECs.
“What if there is a mutation that leads to significantly less leader arm formation? We know these clusters are crucial for neural stem cell migration. By looking at the different phenotypes, we could have an incredible therapeutic investigation,” Matta said.
The team next sought to observe if the effects of vascular cells held true in a substrate similar to brain tissue. However, the common substrate for studying cell migration was unsatisfactorily stiff relative to brain tissue, so Gonzalez’s team was compelled to create a more accurate substrate, a porous biomimetic hydrogel. With the addition of zinc oxide salts to template pores and two abundant brain proteins—fibronectin and laminin—for adherence, the team was able to design a remarkably more brain-like substrate, which allowed for confirmation of their previous results in a pseudo-brain-tissue context.
“Our different materials and different systems that we created specifically for brain migration are novel and can be used for diseases other than stroke and organs other than the brain,” Matta said. “So we really opened up a door for cell migration.”
Having confirmed the pro-clustering behavior of ECs in a brain-like substrate, the team sought to offer a molecular explanation as to why ECs promote NSC clustering. They discovered that ECs secrete an enzyme, matrix metalloproteinase-2, that triggers a protein signaling cascade ultimately leading to cleavage of the cell-cell adhesion protein N-cadherin, a prerequisite for clustering.
The researchers hope that the mechanistic understanding of NSC clustering and migration will help further research on neural tissue regeneration, not just for stroke injuries, but also for other neurological disorders, whose repair mechanisms often feature NSC migration.