Image courtesy of Flickr.
Alzheimer’s disease (AD), the leading cause of dementia affecting fifty-five million people worldwide, is an irreversible neurodegenerative condition marked by progressive memory and cognitive decline due to the loss of neurons and synaptic connections. While conventional AD biomarkers such as beta-amyloid plaques—protein deposits that can interrupt neuronal signaling—are heavily studied, the underlying mechanisms that lead to AD progression have yet to be uncovered. This challenge has compelled researchers to zoom out from research at the neuronal level and start examining other culprits: their astrocyte neighbors, for instance.
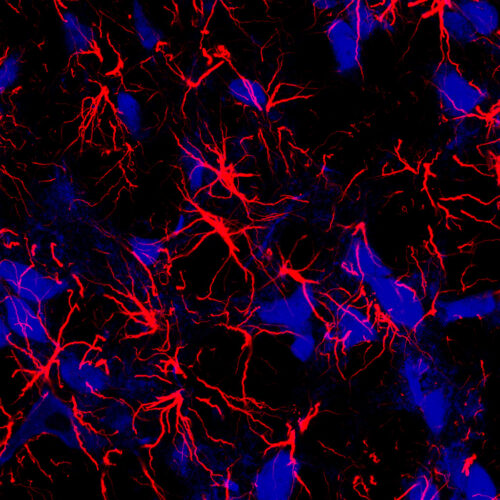
Astrocytes are glial cells, or cells other than neurons in the nervous system, that clear toxic glutamate buildup from the synapse and provide energy to neurons via the biological molecule adenosine triphosphate (ATP). Glial cells outnumber neurons in the brain, but their wide-ranging capabilities have long been overlooked by scientists. For instance, astrocytes contain proteins called brain creatine kinases (CKBs), which transfer a phosphate group from creatine phosphate to form ATP. In a brain with AD, CKBs are oxidized, causing them to undergo a conformational change and become less efficient at ATP production. As a result, this energy deficit coupled with impaired astrocyte function can lead to neuron loss symptomatic of AD.
In a recent study published in Glia, doctoral students Tianyu Zheng and David Kotol worked with professor Jan Mulder at the Karolinska Institutet to elucidate the role of astrocytes in Alzheimer’s disease and identify a new potential biomarker that facilitates early detection of AD.
To do so, the researchers compared CKB availability in brains with AD and Lewy Body dementia (DLB), another condition associated with mental deterioration, to control samples. They used immunofluorescence, a cellular fingerprinting technique, to label various brain cells: neurons, astrocytes, and other glia. Within each sample, CKB was only present in astrocytes. Moreover, there was a significant reduction of antibody binding to CKB in AD samples compared to the DLB and control, suggesting that either less CKB was synthesized or the structure of CKB had changed. Analysis of mRNA expression levels led the researchers to conclude the latter: there was no significant difference in CKB expression in AD samples, so post-translational modifications such as oxidation altered CKB’s affinity for the antibody after protein synthesis.
One unanswered question in AD research is whether a biomarker, like oxidized CKB, is a cause or symptom of neurodegeneration. It is difficult to reconstruct the sequence of events that lead to AD and pinpoint the exact moment a healthy brain progresses into neurodegeneration. To address this issue, Mulder takes inspiration from astronomical methodologies. “Nobody lives long enough to look at the entire life of a star…but if you look at many stars, you’ll find them in different stages of life and death,” Mulder said. Likewise, he proposes sequencing RNA data from cells at different stages of AD to track its developmental trajectory.
In the future, Mulder hopes to verify CKB’s mechanistic interaction with conventional AD biomarkers and synthesize an early detection tool: an antibody specific to the post-translationally modified CKBs. “If you think of Alzheimer’s Disease as a homicide, the neurons are the victims, and the astrocytes are the witnesses,” Mulder said. Through this study, he reminds the scientific community to broaden the focus from examining the neuronal remains at the crime scene and start interrogating the witnesses to uncover the underlying mysteries of AD.