
Myocardial ischemia, or restriction of blood flow to the heart, can cause serious and irreversible damage in cardiac tissue. Now, however, an interdisciplinary team of researchers led by Yale Professor of Medicine, Epidemiology, and Pathology Richard Bucala has developed a group of small molecules that limit the damage that myocardial ischemia causes. Bucala hopes that these molecules will be developed into drugs used to limit ischemia’s detrimental effects.
Myocardial ischemia can have several causes. Heart attack victims suffer from the condition during an attack, and surgeons sometimes intentionally restrict blood flow to the heart during invasive surgeries like coronary bypass. In either case, prolonged ischemia can lead to cell death and permanent damage of the heart muscle, causing abnormal rhythms or reducing the heart’s ability to pump effectively. The molecules designed and tested in several studies by Bucala and his colleagues could potentially prevent some of this damage.

The molecules described in the study target macrophage migration inhibitory factor (MIF), a cytokine cloned by Bucala’s research group that regulates inflammation pathways found in macrophages, endothelial cells, T cells, and cardiomyocytes. In addition to being produced during immune responses, MIF production is stimulated in the heart by lack of oxygen. Bucala and Yale professor Lawrence Young previously collaborated to investigate the role of MIF in responding to ischemic conditions. According to Bucala, “[Young] was very interested to learn that we had mice in which we had genetically knocked out the MIF gene. He was really interested in the role of AMPK [AMP-activated protein kinase] in cardiac ischemia.” In his study, Young found that mouse hearts missing the MIF gene were less able to overcome ischemic injuries. This was due to MIF’s role in activating AMPK by binding to the transmembrane receptor CD74, which initiates a signaling pathway that leads to AMPK activation. AMPK increases glucose uptake and limits apoptosis during ischemia, thereby helping to limit damage to the heart.
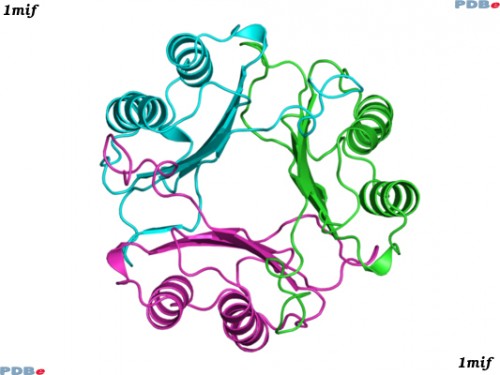
During the time he collaborated with Young, Bucala was also working with Yale professor William Jorgensen to develop small molecule MIF inhibitors that could be used to protect against autoimmune responses. As part of a study originally published in Bioorganic and Medicinal Chemistry Letters in December 2010, Jorgenson and his lab developed computer models of several small molecules using the software BOMB (Biochemical and Organic Model Builder), and synthesized the molecules in the lab. The program, which was developed by Jorgenson, assists with designing small molecules that fit with known structures of protein binding pockets. When assaying the BOMB-designed molecules for MIF inhibition, Bucala and Jorgensen unexpectedly discovered that some of the molecules activated MIF activity. Bucala hypothesizes that these small molecule agonists induce conformational changes that enhance binding between MIF and its receptor.

More recently, Bucala’s team assessed the potential for the agonists’ therapeutic value by assaying the molecules’ effects in in vitro studies on cardiomyocytes and ex vivo studies on mouse hearts, as well as their effects on living mice. Addition of MIF20, the most potent of Jorgenson’s small molecule activators, to mouse cardiomyocytes in vitro increased phosphorylation of AMPK and other downstream effectors. Furthermore, the addition of MIF20 to an ex vivo mouse heart before inducing ischemic conditions improved the heart’s ability to regain a normal heart rate after normal conditions were restored. The addition of MIF20 also increased both glucose oxidation and AMPK activity in post-ischemic conditions. Lastly, mice treated with MIF20 and subjected to localized ischemia around the heart showed less necrosis of heart tissue than mice not treated with MIF20.

Bucala is also working with Yale’s Neurosurgery Department to investigate the use of these molecules to respond to traumatic brain injury. According to Bucala, “We are looking for partners now to develop the agonists.” The group is also hoping in the near future to investigate the small molecules’ therapeutic potential using large mammal models. If they are developed into drug therapies after human trials, the small molecules could be used to limit complications due to heart attacks or restriction of blood flow during surgery.

