In the summer of 2012, physicians at Yale-New Haven Hospital admitted a baby with a mysterious illness. The baby was critically ill with fever and severe diarrhea, yet no infectious agent could be identified and no diagnosis could be made. Turning to powerful genetic tools to unravel this mystery, Yale researchers led by Professors Richard Lifton and Barbara Kazmierczak rapidly zoomed in on a novel mutation in a receptor responsible for initiating the inflammatory response. Thanks to their work, what was once a life-threatening condition that perplexed physicians can now be understood and effectively treated as an autoinflammatory disease.
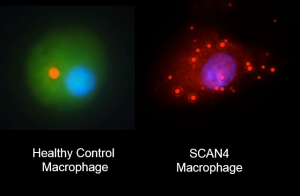
Image Courtesy of Neil Romberg.
The inflammatory response forms an important part of the body’s defense against pathogens. However, it can go out of control, causing the immune system to attack the body’s own cells. This unregulated response was what Dr. Neil Romberg, the paper’s lead author, suspected to be the problem when he saw the baby. Romberg was one of the experts brought in as doctors tried to save the infant, and he saw what he interpreted to be signs of systemic inflammation.
As Romberg attended to the infant, a team led by Lifton “was pulling out all the stops” in sequencing and analyzing the genes of the infant and his parents, Lifton said. In an incredibly short period of five days, they produced a list of genes with de novo mutations in the patient—mutations that were not shared by his parents.
Their efforts initially seemed to have been in vain. “We were disappointed when we looked at the data,” said Lifton, explaining that none of these mutations appeared to be of particular interest. However, when Romberg looked at the sequencing results, his attention was immediately caught by a mutation shared by father and son that affected the inflammatory pathway and had never been seen before. Understanding this mutation took on fresh urgency when, just days later, the father was admitted to intensive care with remarkably similar symptoms. Further study of the family revealed that the mutation was de novo in the father
The mutation in question was in NLRC4, a receptor protein known to play a role in causing inflammation. During an infection, bacterial components and host cell adaptors bind to NLRC4, switching this detector to its active form. In the patient, however, the substitution of one amino acid in this receptor caused it to be stuck in the ‘on’ position. As a result, immune cells containing the mutant protein secreted signaling molecules that set off the inflammatory response even in the absence of pathogens. The blood of the baby and father both had high levels of the signaling molecules that indicated activation of the NLRC4 pathway, providing a link between the gene mutation and abnormal biology in the patients, Strikingly, as Kazmierczak highlighted, these cells also failed to correctly assemble the inflammatory machinery when actually exposed to pathogens, likely impairing the immune response.
Unfortunately, these results did not come in time to save the baby. He died a day before the sequencing analysis was complete. However, armed with insights into the infant’s condition, doctors placed his father on a course of powerful immunosuppressants. It took nine weeks, but the father eventually recovered from a coma and was discharged from hospital.
While the researchers believe that mutations in NLRC4 are likely rare given its detrimental effect on health, they emphasized the need for pediatricians to be aware of this genetic disease, especially given its treatable nature. Remarkably, in the same journal issue in which this study was published, an independent team from the National Institutes of Health reported the case of a patient with similar symptoms who also had a NLRC4 mutation. This concurrence gave the Yale researchers great confidence in their findings. “There is no better biology than another group randomly finding an unrelated patient with the same disease with an independent mutation in the same gene,” said Romberg.
The Yale researchers’ work is a powerful demonstration of how gene sequencing can provide key insights into human disease. With advances in sequencing technology and bioinformatics, diseases that have long confounded physicians may soon be mysterious no more.
