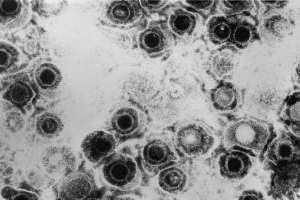
For two billion years, viruses have wreaked havoc on virtually all forms of life. While the public’s attention has been focused on the recent Ebola outbreak in West Africa, common viruses like Herpes Simplex Type II (HSV-2) pose a larger threat of widespread infection throughout the world. According to the CDC, 16.2 percent of all Americans are infected with HSV-2, a rate that has remained steady during the last decade. In August, associate research scientist Norifumi Iijima, Ph.D and Yale Professor of Immunobiology Akiko Iwasaki published a study providing evidence that a network of immune cells residing in the mucosa of the mouse vagina is required for full protection from lethal infection. These findings offer key insights into developing the first HSV-2 vaccine for use in humans.
Most vaccines against viral infection contain weakened or killed viruses. The immune system makes quick business of these easy targets. After this suppressed infection, the body is left with a pool of proteins, known as antibodies, which fit lock-and-key with the virus. When a real infection occurs, those antibodies quickly knock out the intruders and alert a more comprehensive response. Herpes has evolved to counter this defense. Professor Iwasaki explained the difficulties faced in developing a herpes vaccine: “In the case of herpes, because neutralizing antibodies are basically destroyed by the viral coat protein, that strategy is very difficult to implement.”
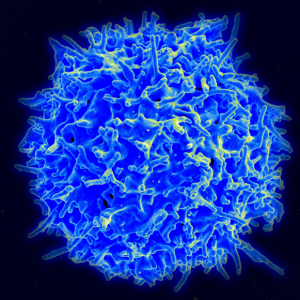
The Iwasaki group has long recognized the old aphorism, “Location, location, location.”The key members of the protective network described in the study are known as CD4 tissue resident (TRM) T cells. They provide a similar sort of “immunological memory” as non-cellular antibodies in the bloodstream, but issue a rapid immune response at the very site of infection. Like the muscle reflex retained in one’s hand after touching a hot stove, these cells react before the rest of the body even recognizes the danger. “Ultimately, we want to apply this to a vaccine,” said Professor Iwasaki. Her group is well known for devising the “prime and pull” paradigm, which recruits circulating CD8 T cells to the vagina to establish CD8 TRM. However, little was previously known about CD4 TRM. This study is critical in understanding how to apply a method similar to “prime and pull” to CD4 cells.
The study demonstrates that CD4 cells converse chemically with macrophages, cells that engulf foreign materials and invaders, in such a way that the CD4 cells maintain a steady-state population. Specifically, the macrophages secrete CCL5, a signaling molecule known as a chemokine. The study indicates that macrophages stimulates CD4 cells to secrete IFN-γ, an antiviral cytokine, that in turn stimulates the macrophages to produce more CCL5. This sequence of events is referred to a as a self-sustaining or “positive feedback loop.” As Iwasaki explained, understanding this maintenance process is only half the battle in applying “prime and pull” to CD4 cells: “We don’t have a good way to establish CD4 memory T cells… [Although] I don’t think it’s a big hurdle.” Furthermore, she cites the challenge of balancing safety with efficacy.
Nevertheless, Iwasaki is used to simultaneously tackling a variety of daunting challenges. She has much to owe to her hands-off style of management, which in turn encourages the creativity of her lab members. “You can’t focus on everything at the same time,” said Iwasaki. “The people in the lab are very independent and self-driven.” This style has enabled her to maintain an impressive record of discovery, even while raising a family. When asked what she looks forward to pursuing, she mentions possibly partnering with a vaccine company to bring her work to the clinical setting. She is also excited about investigating the immunological effects of the “virome,” in particular, the endogenous retroviruses whose precursors are the DNA in our genomes left by viral infections during the course of primate evolution. In her own words, “It’s really cool.”
